| http://magnesiumhilfe.de/poster200009.php, version of: September 9, 2006. |
|
Self-Help Organisation Magnesiumhilfe Poster, September 2000 |
|
Poster at the Ninth International Magnesium Symposium, September 10-15, 2000, Vichy, France The Difficulties in Diagnosis of Magnesium Deficiency by Practitioners from the View of Patients Magnesium-deficiency tetany - the overlooked diseaseD.-H. Liebscher (Berlin), D.-E. Liebscher (Potsdam)
Self-Help Organisation Mineral Imbalances |

|
Magnesium-deficiency tetany is a mostly overlooked disease. It is necessary to sensitise the practitioner for all signs of magnesium deficiency and to implement causal magnesium therapy in handbooks and directives. |
|
Download: (Various systems may not support all formats.) (Gziped Postscript Format - PS, 444kB) (Portable Document Format - PDF, 384kB) |
Both the magnesium-deficiency syndrome [1] as well as the magnesium-deficiency tetany [2] are well described in the literature [3]. However, the implementation of this knowledge in the textbooks for students and practitioners [4] is inadequate. In general, one cannot find sufficient hints to
Magnesium deficiency is defined as an electrolyte metabolic disorder. Although dramatic courses of the disease early in the life are described (in extreme cases the implications of magnesium deficiency are so severe that newborn children would die without high-dosed magnesium therapy [5]), magnesium deficiency is often regarded as a risk factor only and not as the reason of illness. In addition, almost nothing is known among the practitioners about the existence and prevalence of the genetically determined magnesium deficiency. With few exceptions, the experience of the self-help organisation shows that magnesium deficiency finds only inadequate attention in the practical medicine. |
Apparently, this is due to the discrepancy between
There are statements about magnesium that openly contradict expertise. In Germany, magnesium is even classified as controversial medicine [7]. This fatal statement is founded on apparently contradictory results on various questions (myocardial infarction, migraine, headache, diabetes, etc.) This leads to the reproach that many indications exist only in the fantasy of the producers of pharmaceuticals [8]. |
Most of the patients with magnesium deficiency experience an odyssey of many years in being sent from one specialist to the other before the cause of their troubles is found [9]. These patients are always in danger of being classified as hypochondriacs, hysterics, and neurotics. Too often they are correspondingly treated (for instance with cold water gushes). An example: The hyperventilation tetany is better known to the practitioner than the fact that metabolic magnesium deficiency is a wide-spread cause of this tetany [10]. For this reason, patients with hyperventilation tetany are treated more often psychologically and with neuro-pharmaceuticals than with the causal treatment with magnesium instead. In addition, the classification as neurotic is a deadlock trap for all further treatment. But this is not the only problem. Even well diagnosed magnesium-deficiency patients treated with magnesium run the risk that, in case of a necessary hospitalisation, magnesium treatment is stopped because the serum value of magnesium is in the far too wide reference region [9]. This can lead to severe consequences that, nevertheless, are only reluctantly accepted as consequences of magnesium deficiency. The experience of the members of the self-help organisation is that, usually, the illness is diagnosed only 10 to 20 years after the first signs, if the disease is diagnosed at all. Apparently, the reason for that is that the clinical picture of the magnesium-deficiency tetany or the magnesium-deficiency syndrome plays only an insufficient role in medical education. In addition, the prevalence of magnesium deficiency is underestimated. In many manuals the status of magnesium deficiency is described to be very rare. However, it is not rare, and in the differential diagnosis of many illnesses you have to rule it out! In addition, the picture of the magnesium-deficiency syndrome can change during life, and the patient consults different practitioners, the result is an underestimation of the case history. |
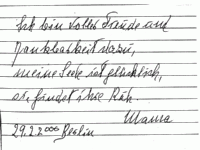
On the left, the writing of a patient (1996) diagnosed as Morbus Parkinson in 1990. The patient began high-dosed substitution of magnesium (1200 mg per diem) in 1998. On the right, the writing of the same patient after 2 years treatment (2000). |
|
Fehlinger wrote with respect to magnesium therapy: It is one of the hardly explicable phenomena in medical history that comparatively simple realisations and progress of often considerable use for the patients are only very slowly propagated and introduced in the everyday routine. Apparently, one obstructing factor is the mere simplicity of the new methods that are comparable to the recommended by Semmelweiss method of washing the hands to limit the childbed fever, a method attacked at its time even by Virchow [11]. |
|